MESI MESI mTABLET ABI / TBI / ECG



For Peripheral Arterial Disease diagnosis, compression and wound healing therapy decision-making.
World’s Fastest Ankle-Brachial Index Screening Device

70% of patients with PAD experience no symptoms and are not diagnosed. Cardiology associations recommend Ankle-Brachial Index screening on complete PAD risk group for early detection of the disease.
*Source: Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II).
Peripheral artery disease (PAD) might seem a relatively contemporary medical phenomena due to its association with unhealthy diet and sedentary lifestyle, among other risk factors, which are increasingly common in population at large. But nothing could be further from the truth as the condition was present in the ancient times, though its pathophysiology was researched much later.

Peripheral Arterial Disease (PAD) — Underdiagnosed and untreated
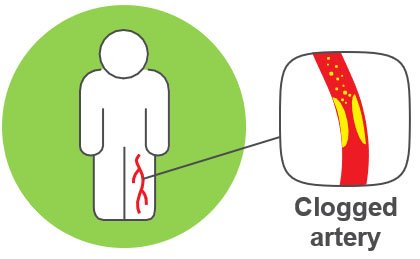
What is Peripheral Arterial Disease (PAD)?
Who is at risk for PAD?
50+
Individuals over 50 years old with cardiovascular
70+
Everyone older than 70
DIABETIC
HYPERTENSIVE
SMOKING
OVERWEIGHT
HIGH CHOLESTEROL
Peripheral Arterial Disease (PAD) is narrowing of the peripheral arteries, most often due to atherosclerosis. It is caused by build-up of plaque in arterial walls. The blood flow is restricted, but the patient does not feel leg pain or other symptoms
PAD is associated with other cardiovascular complications. Its prevalence increases with age. As the world’s populations grow older, so does the number of PAD patients
If not discovered and treated on time, PAD can lead to:
Heart Attack
Stroke
Ulcerations
Amputation
International cardiology associations recommend Ankle-Brachial Index screening for everybody at risk for PAD*
* Source: Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)
Signs & Symptoms
Like many other cardiovascular diseases, PAD is often asymptomatic or presents symptoms, which can be confused with those of other, less or non-serious medical conditions, and is detected only when it is already in a more advanced stage. The most common symptom of PAD is intermittent claudication that often manifests as cramps, numbness and feeling of heaviness (in the legs) during physical exertion.
40%
of individuals with PAD having no symptoms
50%
having symptoms that could be attributed to other medical conditions
*only 10%
having classical PAD symptoms, pain in the legs seems a poor indicator of PAD
* Reference: Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral Arterial Disease Detection, Awareness, and Treatment in Primary Care. JAMA. 2001;286(11):1317–1324. / McGrae McDermott M, Greenland P, Liu K, et al. Leg Symptoms in Peripheral Arterial Disease: Associated Clinical Characteristics and Functional Impairment. JAMA. 2001;286(13):1599–1606.
Diagnosis – A Simple Test to Detect PAD
Diagnosing PAD solely based on outward symptoms is guessing game at best as up to half of PAD patients are entirely asymptomatic. There are far better diagnostic methods, or should we say tools as there are modern medical devices that offer quick identification and estimation of the severity of the disease.
How can PAD be detected?
There are generally two types of diagnostic approaches for PAD; invasive and non-invasive. One method stands out from the others in both the lack of complexity, the need for specialized training and cost-effectiveness when it comes to large scale screening for PAD.
Ankle-Brachial Index (ABI) test is a very simple comparison of blood pressures in legs and arms. It is non-invasive and painless.
ABI = SYSTOLIC BP (ankle) / SYSTOLIC BP (arm)

Traditional Doppler probe measurement
- Takes 30 min
- Hard to perform
- Subjective
- Prone to human error

Automated MESI ABPI MD measurement
- Takes 1 min
- Accurate & objective results
- Simple & saves physician’s time
- Greater physician’s confidence
1. It is a reliable predictor of occlusion of lower extremity arteries – PAD. Detection of PAD is even more important when we know, that over 70% of population is not aware of the occlusions at all.
2. Because of high correspondence of PAD with Coronary Artery Disease (CAD) and Cerebrovascular Disease (CVD), patients diagnosed with PAD have a great chance of early diagnosis of CAD and CVD as well.
ABI screening reference scale
1.41 or more
non-compressible
1.40 – 1.00
normal
0.99 – 0.91
borderline
0.90 – 0.51
abnormal
0.50 or less
severe
Simple ABI measurement procedure
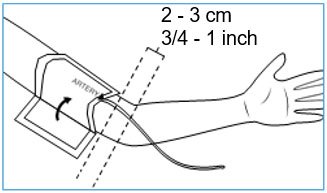
Step 1: Place the arm cuff
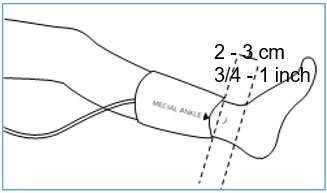
Step 2: Place the ankle cuffs
Simultaneous measurement
1 minute measurement
No human error
Healthcare staff friendly
Report printout
What is Hypertension?

When Systolic Blood Pressure > 140mmHg
Or Diastolic Blood Pressure > 90mmHg
Hypertension is one of the major risk factors for Peripheral Arterial Disease (PAD) and single most important risk factor for stroke. When blood pressure is elevated, muscles in the arteries fight back to manage the pressure. This makes arteries go bigger and arterial wall thicker. The narrowed arteries can develop occlusion, which is a sign for Peripheral Arterial Disease.
How to prevent hypertension?
Don’t smoke
Eat healthy
Be active
Maintain weight
WHY patients with chronic kidney disease need an Ankle–Brachial Index measurement ?
10% of worldwide population is affected by chronic kidney disease

Cross-sectional analysis showed that 24% of patients with chronic kidney disease also have PAD
Patients who are on dialysis and have PAD diagnosis, have 36% higher risk for dying

Over 2 million
people globally currently receive treatment with dialysis or kidney transplantation
Measurement of Ankle–Brachial Index with MESI ABPI MD takes just 1 minute, is non-invasive and offers instant result.

Do you have chronic kidney disease?

You should be evaluated for PAD.
Get ABI measured in 1 minute.
You should know…
According to the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines, patients on dialysis should be all the time evaluated for PAD. Ask your physician for more information!
Diabetes and Peripheral Arterial Disease
Why are Patients with Diabetes at Greater Risk of Pad?
Diabetes is one of the main risk factors for PAD. The risk of developing PAD is proportional to the severity and duration of diabetes. Examples of complications which can lead to PAD in diabetic patients are nerve damage- neuropathy, large blood vessel damage, sudden ischemia of arterial thrombosis and medial artery calcification.
Why do Diabetic Patients Need to be Diagnosed for PAD?
- To identify patients with a high risk of subsequent Myocardial infarction or stroke.
- To elicit and treat the symptoms of PAD that lead to functional disability and limb loss.
- To start therapies that decrease the risk of atherothrombotic events, prevent further diabetic complications and improve the quality of life.a
Who Should Have Their ABI Measured?
- Diabetic patients over 50 years old (if the results are normal, repeated every 5 years).
- Diabetic patients under 50 who have other PAD risk factors (e.g., smoking, hypertension, hyperlipidaemia, or duration of diabetes >10 years).
- All diabetic patients with any symptoms of PAD.
- Every patient who has had diabetes for more than 20 years: patients with type 1 diabetes should have their ABI measured when older than 35 and patients with type 2 should be measured when older than 40 years
